Diabetes is a chronic condition that affects millions of people worldwide. Understanding the differences between Type 1 and 2 diabetes is crucial for effective management and treatment. This blog will cover the key differences, symptoms, causes, and treatments for both types of diabetes, helping you to better understand and manage this condition.
What is Diabetes?
Diabetes is a metabolic disorder characterized by high blood sugar levels. It occurs when the body cannot produce enough insulin or cannot effectively use the insulin it produces. Common symptoms include excessive thirst, frequent urination, and unexplained weight loss.
Understanding Type 1 Diabetes
Causes of Type 1 Diabetes
Type 1 diabetes is an autoimmune condition where the body’s immune system attacks and destroys insulin-producing beta cells in the pancreas. The exact cause is unknown, but genetic factors and environmental triggers, such as viral infections, are believed to play a role.
Symptoms of Type 1 Diabetes
Common symptoms of Type 1 diabetes include:
- Increased thirst and urination
- Extreme hunger
- Unintended weight loss
- Fatigue and weakness
- Blurred vision
Early detection is crucial for managing Type 1 diabetes effectively.
Treatment for Type 1 Diabetes
The primary treatment for Type 1 diabetes is insulin therapy. Patients need to monitor their blood sugar levels regularly and administer insulin through injections or an insulin pump. Additionally, lifestyle adjustments, such as a healthy diet and regular exercise, are essential for managing the condition.
Understanding Type 2 Diabetes
Causes of Type 2 Diabetes
Type 2 diabetes is often associated with lifestyle factors such as obesity and physical inactivity. However, genetics also play a significant role. The body becomes resistant to insulin, and the pancreas cannot produce enough insulin to overcome this resistance.
Symptoms of Type 2 Diabetes
Common symptoms of Type 2 diabetes include:
- Increased thirst and urination
- Increased hunger
- Fatigue
- Blurred vision
- Slow-healing sores
Like Type 1 diabetes, early detection is vital for effective management.
Treatment for Type 2 Diabetes
Treatment for Type 2 diabetes typically includes medications to control blood sugar levels, lifestyle changes such as a balanced diet and regular exercise, and sometimes insulin therapy if other treatments are not effective.
Type 1 and 2 diabetes

Type 1 and type 2 diabetes are both caused by the body’s inability to retain and use glucose, which is required for energy production. This glucose then builds up in the bloodstream and fails to reach the cells that require it, resulting in significant consequences. Type 1 diabetes normally strikes children and adolescents first, although it can strike adults as well. The immune system targets pancreatic beta cells in type 1 diabetes, causing them to stop producing insulin.
Type 1 diabetes cannot be prevented, and it is typically inherited. Type 1 diabetes affects about 5% to 10% of adults with diabetes. Although type 2 diabetes is more common as people get older, it can still strike children. The pancreas makes insulin, but the body is unable to efficiently use it. It appears that lifestyle variables play a role in its development. Type 2 diabetes affects the vast majority of diabetics.
Cardiovascular illness, kidney disease, eyesight loss, neurological problems, and disruption of blood vessels and organs are all consequences of diabetes. Both forms of diabetes are long-term illnesses that impact your body’s ability to manage blood sugar, or glucose.
Type 1 diabetes is characterized by the absence of insulin production. People with type 2 diabetes don’t react to insulin the way they should, and they often don’t produce enough insulin further in the condition. Chronically elevated blood glucose levels can occur in both kinds of diabetes. Diabetes problems are more likely as a result of this.
Tests to Differentiate Type 1 and 2 Diabetes
Common Diagnostic Tests
To differentiate between Type 1 and Type 2 diabetes, doctors use various diagnostic tests, including:
- Blood tests to measure blood sugar levels and HbA1c
- Autoantibody tests to detect immune system markers that attack insulin-producing cells
Interpreting Test Results
Interpreting test results involves looking at the presence of autoantibodies and assessing blood sugar levels. A diagnosis of Type 1 diabetes is likely if autoantibodies are present, while Type 2 diabetes is typically diagnosed based on high blood sugar levels without autoantibodies.
Diabetes Type 1 and 2 Differences
Key Differences in Symptoms
While both types of diabetes share common symptoms, some unique signs help differentiate them:
- Type 1 Diabetes: Rapid onset of symptoms, often in childhood or adolescence.
- Type 2 Diabetes: Gradual onset of symptoms, usually in adulthood.
Differences in Causes
- Type 1 Diabetes: Primarily caused by genetic and autoimmune factors.
Type 2 Diabetes: Linked to lifestyle factors such as diet, physical inactivity, and obesity, along with genetic predisposition.
How to Differentiate Type 1 and 2 Diabetes
Clinical Diagnosis
A doctor’s assessment is essential for accurately diagnosing the type of diabetes. This includes a thorough medical history, physical examination, and interpretation of diagnostic tests.
Self-Assessment Tips
Patients can monitor their symptoms and risk factors to get an early indication of diabetes. Persistent symptoms such as extreme thirst, frequent urination, and unexplained weight loss should prompt a visit to the doctor.
Managing Diabetes Effectively
Importance of Early Diagnosis
Early diagnosis of diabetes can significantly improve treatment outcomes and prevent complications. It allows for timely intervention and better management of the condition.
Lifestyle Changes for Management
Lifestyle changes play a crucial role in managing diabetes. These include:
- Diet: Eating a balanced diet rich in whole grains, fruits, vegetables, and lean proteins.
- Exercise: Regular physical activity to help control blood sugar levels and maintain a healthy weight.
- Monitoring: Regularly checking blood sugar levels to ensure they are within the target range.
What is Type 1 Diabetes
If you have type 1 diabetes, you’ll require insulin to keep your blood sugar levels in check. You should also monitor your blood sugar levels on a regular basis. Also, keep track of how many carbs (carbohydrates) you consume. Monitoring your carbs will assist you in determining how much insulin you should inject with your meals.
You should also aim to have a healthier diet in general. This includes frequent physical activity as well as a nutritious, well-balanced diet. These will assist you in lowering your chances of developing diabetes problems.
Type 1 diabetes has a number of causes.
The immune system is in charge of defending the body against outside attackers such as dangerous viruses and bacteria. The immune system misidentifies the body’s natural healthy cells as unwanted intruders in individuals with type 1 diabetes. The pancreas’ insulin-producing beta cells are attacked and destroyed by the immune system. The body is incapable of manufacturing insulin if these beta cells are not there.
What is Type 2 Diabetes
You must also consume a nutritious diet and exercise if you have type 2 diabetes. These items will aid in the management of your obesity and diabetes.
People with type 2 diabetes, on the other hand, frequently require medications. Tablets and insulin, for example, as well as other treatments are available. The treatment you’re on will determine if you need to test your blood sugar levels like someone with type 1.
Type 2 diabetes has a number of causes.
Insulin resistance is a symptom of type 2 diabetes. Although the body continues to manufacture insulin, it is unable to utilize it properly. Many people are still puzzled as to why some people become insulin resistant while others do not, but various lifestyle modifications, such as inactivity and obesity, may play a role.
Other environmental and genetic variables could be at play. Your pancreas will try to make up for type 2 diabetes by generating extra insulin. Since your body is unable to utilize insulin adequately, glucose builds up in your bloodstream.
Symptoms of Type 1 and Type 2 Diabetes
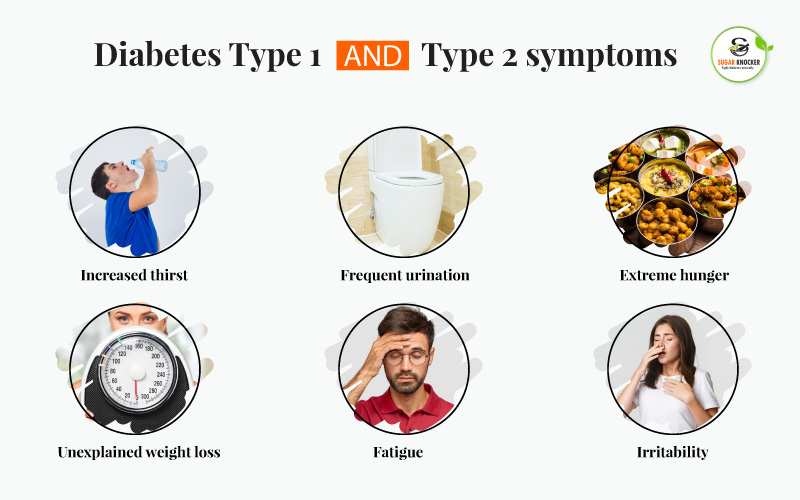
Diabetes is a serious condition, and due to poorly controlled blood sugar, a diabetic may have negative sensations. But the question is which form of diabetes is worse: Type 1 or type 2?
Excess weight, high blood pressure, and cardiovascular disease are all symptoms of metabolic syndrome, which can occur alongside type 2 diabetes.
Symptoms of type 1 and type 2 diabetes are similar. They are as follows:
| Type 1 Symptoms | Type 2 Symptoms |
| Excess thirst | Excess thirst |
| Increased Urination | Increased Urination |
| Excess hunger | Excess hunger |
| Feeling of tiredness and fatigue at all times | Feeling of tiredness and fatigue at all times |
| Hazy Eyesight | Hazy Eyesight |
| Numb hands and feet | Numb hands and feet |
| Slow-healing wounds | Slow-healing wounds |
| Sudden weight loss | Sudden weight loss |
However, the appearance of type 1 and type 2 diabetes symptoms differs. Type 1 can reveal itself quickly. This makes them more difficult to dismiss. This is critical since untreated symptoms might lead to diabetic ketoacidosis (DKA).
Type 2 diabetes, on the other hand, is more difficult to detect. This is due to the fact that it develops more slowly, particularly in its early phases. This makes detecting the signs more difficult. That is why knowing your risk of acquiring type 2 diabetes is crucial. Some people are diabetic and are completely unaware of it. They can keep it for up to ten years without being aware of it.
Risk factors for type 1 and type 2 diabetes
Both type 1 and type 2 diabetes can be caused by genetic and environmental causes. Many people, however, may be able to prevent type 2 diabetes by leading a balanced lifestyle.
Type 1 diabetes has a number of risk factors:
- having a diabetes family history
- having particular genetic characteristics that affect how the body generates or uses insulin
- infection or virus exposure, such as mumps or rubella cytomegalovirus
Some medical diseases, such as cystic fibrosis or hemochromatosis, induce a type of diabetes that is remarkably similar to type 1 diabetes by reducing the person’s insulin production.
The following are some of the risk factors for type 2 diabetes:
- having a type 2 diabetic in the family
- having a problem with obesity
- smoking
- consuming an unfit diet
- a lack of activity
- the use of certain drugs, such as HIV meds and chronic steroids
Diagnosis for Type 1 and Type 2 Diabetes
The development of type 1 diabetes is usually abrupt. If a person experiences symptoms, they should seek medical attention as soon as possible.
A person with type 2 diabetes in its initial stages, on the other hand, may have no symptoms. A normal blood test, however, will reveal high blood sugar levels at this point.
Obese people and others who are at risk for type 2 diabetes ought to have their glucose concentrations checked on a regular basis. They may have diabetes or prediabetes if their blood sugar levels are high.
Prediabetes is a condition in which a person’s blood sugar levels are elevated but not elevated enough to be detected with type 2 diabetes.
The tests listed below can help identify type 1 or type 2 diabetes, however not all of them are appropriate for both:
- A1C test: An A1C test involves a doctor taking a blood sample to determine a person’s normal blood glucose level over the previous 2-3 months.
- The fasting plasma glucose (FPG) test determines a person’s blood sugar levels after they have fasted for a period of time. Patients must fast for at least 8 hours before the test, therefore many people take it before breakfast.
- The oral glucose tolerance test (OGTT) assesses a person’s ability to digest glucose. A patient will be given a blood glucose test two hours before and after consuming a sugary beverage.
- RPG test: A doctor will perform an RPG test to determine a person’s blood sugar levels level at any time during the day. This test does not need a patient to fast prior to taking it.
The chart below indicates which test findings suggest diabetes:
| A1C (mg/dl) | OGTT (mg/dl after 2 hours) | RPG (mg/dl) | FPG (mg/dl) | |
| Diabetes | 6.5% or above | 200 or over | 200 or over | 126 or over |
| Prediabetes | 5.7–6.4% | 140-199 | 100-125 | |
| Normal | below 5.7% | Below 140 | Below 200 | Below 100 |
It is advised that patients aged 45 and up to be screened for type 2 diabetes on a routine basis. Younger people who are more at risk of developing diabetes, such as those with a family history of the disease, should be tested for type 2 diabetes on a frequent basis.
At home, people can monitor their blood sugar levels. A person who does not have diabetes but is concerned about readings from a home test should see their doctor.
Cure and Prevention of Type 1 and Type 2 Diabetes

It is impossible to prevent type 1 diabetes.However, by making the following lifestyle changes; you may be able to reduce your risk of acquiring type 2 diabetes:
- maintain a healthy weight
- If you are overweight, consult with your doctor to design a healthy weight-loss strategy.
- raising your amount of physical activity
- consuming a well-balanced diet and limiting sugary and highly processed foods
Even if you can’t prevent the condition from occurring, diligent monitoring can help you get your blood sugar levels back to normal and avoid significant problems. There’s proof that decreasing weight can help some people with type 2 diabetes go into remission. You can put your type 2 diabetes into remission by following an extremely low-calorie diet under the doctor’s supervision or undergoing surgery.
Treatment for type 1 and type 2 diabetes
There is no cure for diabetes, but treatment can help people manage the condition and prevent it from worsening. Here are some points about treating and managing diabetes.
Gastric bypass surgery, lifestyle changes, and medication can result in the remission of type 2 diabetes.
| Type 1 | Type 2 | |
| Possible cure | -There is presently no cure, but medication can assist in managing symptoms over time. -Gene therapy, regenerative medicine with stem cells, and pancreatic islet transplantation are all being explored as potential treatment options. | -While there is no treatment at this time, there are ways to halt the disease’s development and manage the symptoms.- Overweight and obese individuals may benefit from a gastric bypass. |
| Treatment with Insulin and other drugs | -Frequent insulin injections or an insulin pump can supply insulin as requiredduring the course of the day. -Other drugs, such as pramlintide, can help keep blood glucose levels in check. |
– Metformin can lower the quantity of sugar produced by the liver.– Blood sugar levels can be reduced by using SGLT2 inhibitors, DPP-4 inhibitors, or alpha-glucosidase inhibitors.- Insulin levels can be raised using meglitinides or sulfonylureas. – Thiazolidinediones can improve insulin sensitivity. – Glucagon-like peptide-1 agonists can raise insulin levels while lowering blood sugar levels. – Amylin analogs inhibit digestion, which helps to lower blood sugar levels. – Insulin may be beneficial in some circumstances. |
| Lifestyle treatments | -Stick to a treatment plan and seek medical guidance if necessary.-Live a healthy, active lifestyle.-When exercising, keep an eye on your glucose levels.-Keep your blood pressure and cholesterol levels in check. | -Stick to a treatment plan and seek medical guidance if necessary.-Live a healthy, active lifestyle.-Keep blood pressure and cholesterol levels in check.-Refrain from smoking- Be aware of the warning indications of side effects and problems. |
| Avoiding Complications | -Stick to the treatment plan.-Recognize the indicators of hypoglycemia and hyperglycemia.-Keep a medical ID on you at all times.-Take precautions to prevent infection-Have regular eye exams-Check for wounds and seek treatment as soon as possible. Type 1 diabetes cannot be prevented at this time. |
-Be aware of the warning signals of potential issues -Carry a medical ID -Take precautions to avoid infections -Check for wounds and get treatment as soon as possible -Have regular eye exams -Eat a healthy diet and exercise regularly -Eat a balanced diet and exercise regularly- Avoid or quit smoking and follow a doctor’s advice if prediabetes is diagnosed. |
Conclusion
Understanding the differences between Type 1 and Type 2 diabetes is essential for effective management and treatment. While both types share common symptoms, they have distinct causes, diagnostic methods, and treatment approaches. Type 1 diabetes is primarily an autoimmune condition, often diagnosed in childhood, requiring lifelong insulin therapy. In contrast, Type 2 diabetes is often associated with lifestyle factors and typically occurs in adults, manageable with lifestyle changes and medication
Diabetes is a dangerous disease, and it is something you should never ignore because it can develop into something even more serious. Although there is no way you can prevent type 1 diabetes, insulin and other medications can help you in managing symptoms.
While both types of diabetes may have a hereditary component, people can lower their risk of type 2 diabetes and manage its progression by leading a healthy, active lifestyle. Anyone who has been diagnosed with prediabetes should adopt a healthy lifestyle to eliminate or reduce the risk of acquiring type 2 diabetes.
For more information on diabetes management, symptoms, and treatment options, explore our related blog posts and resources.