Diabetics are at a higher risk for foot problems due to the nerve damage, circulation problems and longer healing times which are associated with long term diabetes and high sugar levels. Many a times, they are not able to accurately judge the damage to their feet and can neglect them till too late. At the same time, impaired circulation and compromised immune system increase the time any wound takes to heal.
Therefore, it is important for diabetics to take regular and good care of their feet on a day-to-day basis and also to avoid injury or infections.
What Causes Diabetes-Related Foot Conditions?
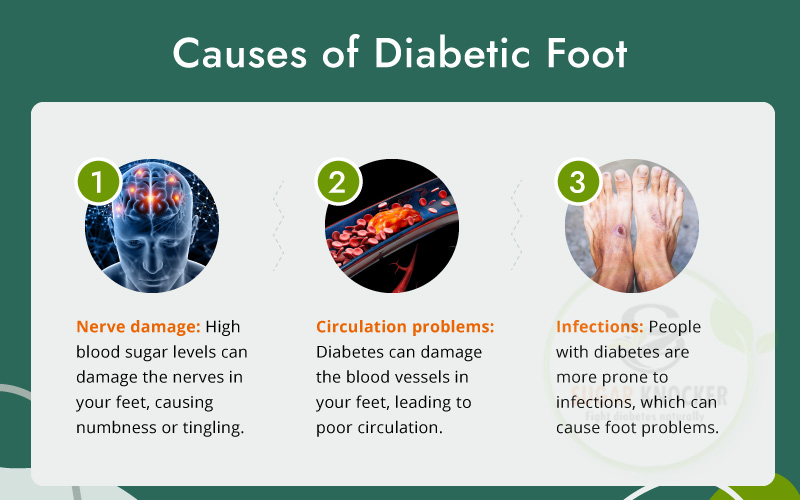
Diabetes-related foot conditions can occur due to a combination of factors associated with diabetes, including nerve damage (neuropathy), poor blood circulation, and immune system suppression.
When blood sugar levels are high, it can lead to nerve damage, particularly in the feet, which can result in decreased sensation, making it difficult to notice cuts, sores, and other foot injuries. Without proper care, these injuries can lead to infections, ulcers, and even gangrene, which may eventually require amputation.
Poor blood circulation also contributes to diabetes-related foot problems. High blood sugar levels can damage blood vessels, leading to reduced blood flow to the feet. As a result, foot injuries may not heal properly, and infections may not be fought off efficiently.
Moreover, diabetes can weaken the immune system, which can increase the risk of infection in the feet. When combined with poor circulation and nerve damage, infections can be particularly difficult to treat and can lead to serious complications.
1)Nerve damage: High blood sugar levels can damage the nerves in your feet, causing numbness or tingling.
2)Circulation problems: Diabetes can damage the blood vessels in your feet, leading to poor circulation.
3)Infections: People with diabetes are more prone to infections, which can cause foot problems.
4)Wound healing problems: High blood sugar levels can also slow down the healing process, making it difficult for wounds or injuries to heal.
How are diabetes-related foot conditions diagnosed?
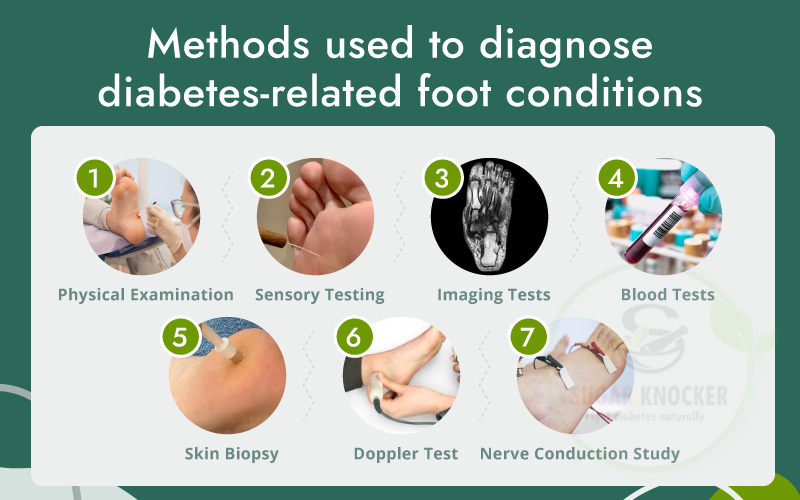
There are several diabetes-related foot conditions that can be diagnosed through a combination of physical examination and various diagnostic tests. Here are some of the most common methods used to diagnose diabetes-related foot conditions:
Physical Examination:
During a physical examination, the doctor will visually inspect your feet for any signs of injury, infection, or deformities. They may also check for areas of numbness or tingling, as well as assess the circulation in your feet.
Sensory Testing:
A doctor may also perform sensory testing to check for nerve damage. This can be done through a monofilament test, which involves touching a thin nylon filament to various parts of the foot to see if the patient can feel it.
Imaging Tests:
Imaging tests, such as X-rays, MRI scans, or ultrasounds, can be used to detect any bone fractures, soft tissue damage, or deformities.
Blood Tests:
Blood tests can be used to measure blood glucose levels, which can help diagnose diabetes-related foot conditions.
Skin Biopsy:
A skin biopsy may be taken to help diagnose skin infections or to assess the presence of foot ulcers.
Doppler Test:
This test helps to determine blood flow in the foot and ankle, using high-frequency sound waves to measure the speed and direction of blood flow in arteries and veins.
Nerve Conduction Study:
This test measures how quickly electrical signals travel through the nerves in the foot, helping to diagnose peripheral neuropathy.
The specific tests used will depend on the individual’s symptoms and the suspected condition. It’s important to consult a doctor if you experience any foot-related symptoms as early diagnosis and treatment can help prevent serious complications.
Symptoms of Diabetic Foot

Diabetic foot is a complication of diabetes that affects the feet. It is caused by nerve damage and poor circulation in the feet, which can lead to serious foot problems. The symptoms of diabetic foot can include:
- Numbness or tingling in the feet.
- Loss of sensation in the feet.
- Slow-healing sores or wounds on the feet.
- Redness, swelling, or warmth in the feet.
- Foul-smelling discharge from a wound or sore.
- Burning or stabbing pain in the feet.
- Cuts, sores, or blisters that do not heal.
- Skin discoloration or temperature changes.
- Ingrown toenails or fungal infections.
If diabetes-related neuropathy leads to foot ulcers, symptoms to watch out for include:
- Any changes to the skin or toenails, including cuts, blisters, calluses or sores.
- Discharge of fluid or pus.
- Foul smell.
- Pain.
- Redness.
- Skin discoloration.
- Swelling.
[Also Check Why, How and When Diabetic Face Amputations?]
Healthy Foot Habits To Follow:

Taking care of your feet is important for maintaining overall health and well-being. Here are some healthy foot habits you can practice:
Wash your feet regularly:
Clean your feet daily with soap and warm water to prevent bacteria and odors.
Keep your feet dry:
Moisture can lead to fungal infections, so make sure to dry your feet thoroughly after washing or sweating.
Wear comfortable shoes:
Choose shoes that fit well and provide support. Avoid wearing shoes that are too tight or too loose.
Alternate your shoes:
Alternate between different pairs of shoes to allow them to dry out and reduce wear and tear.
Trim your toenails regularly:
Trim your toenails straight across to prevent ingrown nails.
Moisturize your feet:
Keep your feet soft and smooth by applying a moisturizer or foot cream.
Exercise your feet:
Stretch and exercise your feet and ankles regularly to improve flexibility and prevent injury.
Get regular foot check-ups:
Visit a podiatrist for regular foot check-ups, especially if you have diabetes or other health conditions that can affect your feet.
By practicing these healthy foot habits, you can keep your feet happy and healthy.
Prevention of Diabetic Foot:
Preventing diabetic foot is essential for people with diabetes. Here are some steps that can be taken to prevent diabetic foot:
Inspect your feet every day
Look for sores, redness, blisters, cuts, bunions, corns or bruises all along the sides of your feet, soles and in between the toes. Use a mirror or ask for help if you are unable to inspect them properly. Contact your doctor immediately if you see any of the above symptoms and track their healing.
Use good quality footwear and socks
Make sure to buy shoes or sandals that fit your feet properly and cover them all around. They should not pinch in any place nor make your feet sore. It is advisable to cover your feet at all times, even when at home. Always inspect shoes before wearing to ensure there are no objects inside.
[Also Check Diabetic Ulcers on Foot and Treatment]
Wash and moisturize feet daily
Maintain good foot hygiene. Wash them daily and make sure to dry them properly, especially between the toes. Moisturize feet, except between the toes, to avoid dry and cracked feet.
Following these tips along with your regular diabetes management plan to control sugar levels will go a long way in avoiding serious foot trouble.
Keep feet clean and dry
Keeping the feet clean and dry is essential to prevent infections and reduce the risk of complications. Excess moisture can lead to fungal infections, while cuts or wounds can become infected if not kept clean. Additionally, diabetics should avoid exposing their feet to extreme temperatures and should inspect their feet daily for any cuts, blisters, or sores. Keeping feet clean and dry can help prevent infections and reduce the risk of developing sores.
Quit smoking
Diabetes is a condition that affects the body’s ability to regulate blood sugar levels. When a person with diabetes smokes, it can damage their blood vessels, reducing blood flow to their feet. This can lead to a higher risk of developing foot infections, which can be particularly dangerous for people with diabetes.
Foot infections can progress rapidly in people with diabetes and can lead to serious complications such as gangrene and amputation. Therefore, quitting smoking is essential for people with diabetes to reduce their risk of developing foot infections and other related complications.
How are diabetes-related foot ulcers treated?

Diabetes-related foot ulcers are usually treated with a combination of medical and surgical interventions. The primary goal of treatment is to heal the wound and prevent it from becoming infected or developing into a more serious condition such as gangrene.
Here are some common treatments for diabetes-related foot ulcers:
Wound care:
The wound is cleaned and dressed regularly to keep it moist and prevent infection.
Offloading:
Pressure is taken off the affected foot with the use of special shoes or boots, or by using crutches, a walker, or a wheelchair. This helps to reduce the pressure on the ulcer and promote healing.
Debridement:
Dead or infected tissue is removed from the ulcer to promote healing.
Antibiotics:
If the ulcer is infected, antibiotics may be prescribed to treat the infection.
Surgery:
In some cases, surgery may be necessary to remove dead tissue or to reconstruct the affected area.
Blood sugar control:
Tight control of blood sugar levels can help to prevent further damage to the affected foot and promote healing.
Nutritional support:
A balanced diet with adequate protein and vitamins is important for healing.
It is important to seek medical attention promptly if you develop a foot ulcer, as early treatment can help prevent serious complications.
When is the right time to visit doctor:

- Check your feet every day for any signs of cuts, blisters, sores, or changes in skin color or temperature.
- Pain in feet or Loss of sense.
- If you have a cut, blister, or sore on your foot that isn’t healing.
- If you notice any signs of fungus infection on your feet.
- If any infections or cuts in between the toes.
- If found any foot ulcer.
- Deep cracks on feet.
Conclusion:
Diabetic foot is a serious condition that can cause significant pain and discomfort. It is caused by a combination of factors related to the effects of diabetes on the body, including peripheral neuropathy and poor circulation. Preventing diabetic foot is crucial for people with diabetes, and there are several steps that can be taken to reduce the risk of developing this condition. If you have diabetes and notice any changes in your feet, speak to your healthcare provider as soon as possible to prevent complications.
Remember with diabetes prevention is not just the best, but the only option!