The Unseen Spikes – Why PPBS Matters More Than You Think
Have you ever diligently monitored your blood sugar, felt a sense of relief with a good fasting reading, only to find yourself wondering why your diabetes still feels so challenging? You’re not alone. Many individuals with diabetes, and even those at risk, are increasingly focusing on a crucial, yet often overlooked, aspect of blood sugar control: Post-Prandial Blood Sugar (PPBS).
It’s shedding light on the hidden spikes in blood sugar that occur after meals, which can have profound implications for long-term health. This growing awareness is a powerful step towards more effective diabetes management.
This blog post will be your comprehensive guide to understanding PPBS. We’ll delve into what it is, why it holds such immense importance in diabetes, how to accurately monitor it, and most importantly, equip you with practical and effective strategies to keep your post-meal blood sugar in check for a healthier, more vibrant life.
What Exactly is Post-Prandial Blood Sugar (PPBS)?
Let’s start with the basics. Post-Prandial Blood Sugar (PPBS) refers to the level of glucose (sugar) in your blood after you’ve consumed a meal. The term “post-prandial” simply means “after a meal.”
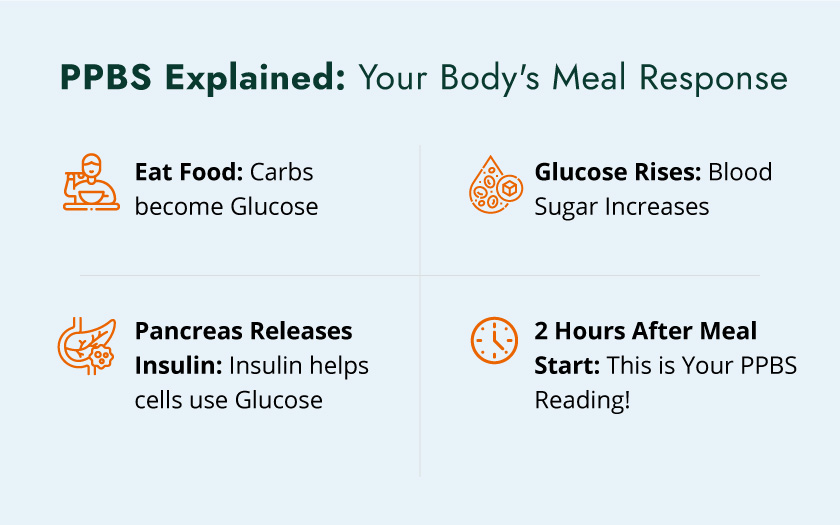
The Body’s Glucose Journey After a Meal:
When you eat, especially foods rich in carbohydrates, a fascinating process begins in your body:
- Digestion: Carbohydrates, whether from a plate of rice, a roti, or a fruit, are broken down into simpler sugars, primarily glucose, in your digestive system.
- Absorption: This glucose is then absorbed into your bloodstream from your small intestine, causing your blood sugar levels to rise.
- Insulin’s Role: In response to this rise in blood sugar, your pancreas, a vital organ located behind your stomach, releases a hormone called insulin. Insulin acts like a key, unlocking your body’s cells (muscle, fat, and liver cells) to allow glucose to enter and be used for energy or stored for later.
- Blood Sugar Normalization: As glucose moves into your cells, your blood sugar levels begin to decrease, ideally returning to a healthy range within a few hours.
Different macronutrients influence PPBS differently:
- Carbohydrates: Have the most direct and immediate impact on PPBS as they are readily converted to glucose.
- Proteins: Have a minimal direct impact on immediate PPBS, but can cause a delayed, smaller rise in blood sugar due to gluconeogenesis (conversion of protein to glucose).
- Fats: Generally have a very minimal direct impact on blood sugar but can slow down gastric emptying, potentially delaying and sometimes prolonging the post-meal glucose rise.
The “Post-Prandial” Window:
While blood sugar levels fluctuate constantly, the PPBS test is typically measured 2 hours after the start of a meal. This specific timing is crucial because it allows enough time for the ingested food to be digested and absorbed, and for your body’s insulin response to try and manage the glucose influx. It provides a snapshot of how efficiently your body is processing the carbohydrates from that particular meal. In some cases, particularly for diagnosing gestational diabetes, a 1-hour post-meal test might also be performed.
Distinguishing PPBS from Other Blood Sugar Tests:
It’s important to understand how PPBS fits into the broader picture of blood sugar monitoring:
Fasting Blood Sugar (FBS):
This test measures your blood glucose levels after an overnight fast (typically 8-12 hours). It tells you your baseline blood sugar without any recent food intake. While important, a normal FBS doesn’t guarantee overall good blood sugar control, as it doesn’t reflect how your body handles food.
Discover 8 proven tips to reduce high fasting sugar levels
HbA1c (Glycated Hemoglobin):
This test provides an average of your blood sugar levels over the past 2 to 3 months. It’s a fantastic long-term indicator of diabetes control. However, HbA1c can sometimes mask significant post-meal spikes if your fasting numbers are consistently low. Elevated PPBS can significantly contribute to a higher HbA1c, even if your fasting numbers appear “normal.”
Random Blood Sugar (RBS):
This is a blood sugar test taken at any random time, regardless of when you last ate. While useful for immediate checks, it’s less specific than FBS or PPBS for understanding glucose metabolism in relation to meals.
In essence, while FBS and HbA1c offer crucial insights, PPBS provides a dynamic view of your body’s immediate response to food, making it an invaluable tool for precise diabetes management.
Why is PPBS So Important in Diabetes Management?
The significance of PPBS extends far beyond just numbers. It provides critical insights into how your body manages food intake, and its uncontrolled fluctuations can have serious long-term consequences for your health.
Beyond the Fasting Number: The Unseen Spikes
Imagine checking your fasting blood sugar in the morning and seeing it perfectly within the normal range. It’s a great feeling! However, this single reading doesn’t reveal what happens after you eat. For many individuals, especially those with prediabetes or early-stage diabetes, their fasting glucose might be well-controlled, but their blood sugar can soar significantly after meals. These “unseen spikes” can silently contribute to health complications over time, making PPBS a vital metric for truly understanding your metabolic health.

Early Detection of Prediabetes and Diabetes:
Elevated PPBS levels can be an early warning sign, often appearing before fasting glucose levels become high enough for a diabetes diagnosis. If your 2-hour PPBS is consistently between 140 mg/dL and 199 mg/dL, it indicates impaired glucose tolerance or prediabetes. This is a critical window of opportunity for intervention. By addressing these elevated post-meal levels, you can significantly delay or even prevent the progression to full-blown Type 2 Diabetes. For individuals in India, where the prevalence of diabetes is high, early detection through PPBS can be particularly impactful.
Impact on Long-Term Complications:
Persistent high PPBS, even if fasting levels are seemingly normal, is a major contributor to various diabetes complications:
Cardiovascular Disease (CVD):
High post-meal glucose spikes are strongly linked to an increased risk of heart disease, stroke, and damage to blood vessels. These spikes contribute to oxidative stress, a process that harms cells and tissues, leading to inflammation and plaque buildup in arteries. This can result in conditions like atherosclerosis (hardening of the arteries), increasing the risk of heart attacks and strokes.
Microvascular Complications:
These are complications affecting the small blood vessels:
Retinopathy (Eye Damage):
High blood sugar can damage the tiny blood vessels in the retina, leading to vision problems and, if left untreated, even blindness.
Neuropathy (Nerve Damage):
Elevated glucose levels can harm nerves throughout the body, leading to numbness, tingling, pain, especially in the feet and hands, and can also affect organ function (autonomic neuropathy).
Nephropathy (Kidney Damage):
The delicate filtering units in the kidneys can be damaged by consistently high blood sugar, potentially leading to kidney disease and even kidney failure.
Contribution to HbA1c:
While HbA1c gives an average, significant post-meal spikes directly contribute to a higher overall HbA1c value. Effectively managing PPBS is therefore crucial for achieving your target HbA1c goals and reducing your overall risk of complications.
Personalized Treatment and Dietary Adjustments:
PPBS readings provide invaluable real-time feedback that empowers both you and your healthcare team. By understanding how specific meals, activities, and medications affect your blood sugar after eating, your doctor can:
- Fine-tune your medication dosages (especially insulin or certain oral medications).
- Recommend specific dietary modifications, helping you identify trigger foods.
- Advise on the timing of meals and exercise.
In essence, PPBS acts as a personalized roadmap, guiding you towards more effective and tailored diabetes management.
Understanding PPBS Ranges: What Do Your Numbers Mean?
Once you have your PPBS readings, it’s natural to wonder what they signify. Understanding the different ranges is key to interpreting your results and making informed decisions about your health. Keep in mind that specific target ranges can vary based on individual health conditions, age, and your doctor’s recommendations.
Normal PPBS Ranges (for non-diabetic individuals):
For individuals without diabetes, the body efficiently manages blood sugar spikes after a meal.
- Typically, PPBS should be less than 140 mg/dL (or 7.8 mmol/L) two hours after the start of a meal.
- Blood sugar usually peaks around 60 minutes after eating and then returns to pre-meal levels within 2-3 hours. In India, the general guideline for a normal PPBS test is 70-140 mg/dL for healthy individuals.
Prediabetes PPBS Ranges:
If your 2-hour PPBS falls within this range, it’s a significant indicator of prediabetes or impaired glucose tolerance:
- PPBS between 140 mg/dL and 199 mg/dL (7.8 mmol/L to 11.0 mmol/L) two hours after a meal. This range signifies that your body is having trouble processing glucose effectively after meals, putting you at a higher risk of developing Type 2 Diabetes. This is a crucial opportunity to implement lifestyle changes to prevent progression.
Diabetes PPBS Ranges:
For individuals diagnosed with diabetes, these are the typical ranges that indicate uncontrolled or managed blood sugar:
- PPBS of 200 mg/dL (11.1 mmol/L) or higher two hours after a meal suggests diabetes.
- For individuals with diagnosed diabetes, the target PPBS is often recommended to be less than 180 mg/dL (10.0 mmol/L) two hours after a meal. However, this target can be individualized by your doctor based on factors like age, other health conditions, and risk of hypoglycemia. Always discuss your personal target ranges with your healthcare provider.
Factors Influencing PPBS Readings (Beyond Meals):
While your meal is the primary driver of PPBS, several other factors can influence your readings:
- Medications: Certain medications, even those not directly for diabetes (e.g., steroids, some diuretics, beta-blockers), can affect blood sugar levels. Always inform your doctor about all medicines you are taking.
Physical Activity:
Exercise can significantly lower blood sugar by increasing insulin sensitivity and glucose uptake by muscles. The timing and intensity of activity around meals can impact PPBS.
Stress and Illness:
Emotional stress and physical illness (like infections) can trigger the release of hormones that raise blood sugar levels, even if you haven’t eaten much.
Hydration:
Dehydration can sometimes lead to artificially higher blood sugar readings.
Meal Composition:
The type and quantity of carbohydrates are paramount, but also the amount of fat and protein can influence the rate of glucose absorption and thus the PPBS peak. For instance, a high-fat meal might delay the peak but keep blood sugar elevated for longer.
Gastric Emptying Rate:
How quickly food moves from your stomach to your small intestine can affect how rapidly glucose enters your bloodstream.
Insulin Sensitivity:
This refers to how effectively your body’s cells respond to insulin. Higher insulin sensitivity means cells readily take up glucose, leading to lower PPBS.
Understanding these variables helps you and your doctor interpret your PPBS readings more accurately and develop a tailored management plan.
The PPBS Test: Procedure and Preparation
The PPBS test is a straightforward blood test, but precise preparation is essential to ensure accurate results.
Who Needs a PPBS Test?
Your doctor might recommend a PPBS test if you:
Exhibit symptoms of high blood sugar:
Such as increased thirst, frequent urination, unexplained weight loss, fatigue, or blurred vision.
Are at risk for diabetes:
This includes individuals with a family history of diabetes, obesity, high blood pressure, high cholesterol, or a history of gestational diabetes.
Have been diagnosed with diabetes:
It’s a crucial tool for monitoring your current treatment plan and making necessary adjustments.
Are pregnant:
To screen for or monitor gestational diabetes.
Experience reactive hypoglycemia:
Where blood sugar drops too low a few hours after eating.

How the Test is Performed:
The standard PPBS test procedure typically involves these steps:
Fasting Blood Sample (Optional but common):
In many cases, your doctor might first request a fasting blood sugar (FBS) test. This requires you to fast for 8-12 hours beforehand (usually overnight). This provides a baseline glucose level before any food intake.
The “Challenge Meal”:
After the fasting blood sample (if collected), you will be instructed to consume a specific meal. This is often a standardized glucose solution containing 75 grams of carbohydrates (similar to an Oral Glucose Tolerance Test – OGTT) or a regular meal that you would typically eat. It’s crucial to follow your doctor’s instructions regarding this meal.
The Waiting Period:
Once you start eating your meal, a timer begins. You will need to wait for exactly two hours. During this time, you should avoid any strenuous physical activity, smoking, or consuming any food or drinks other than plain water.
Second Blood Sample Collection:
Exactly two hours after you started your meal, a second blood sample will be drawn from a vein, typically in your arm. This sample measures your post-prandial blood sugar.
Crucial Preparation Steps for Accurate Results:
Adhering to these preparation guidelines is paramount for obtaining reliable PPBS test results:
Fasting (if required):
If your doctor has requested a fasting blood sugar test alongside your PPBS, ensure you adhere to the 8-12 hour fasting period (no food or drinks except water).
Standardized vs. Regular Meal:
If a specific meal is prescribed (e.g., a glucose solution), do not deviate from it. If you’re instructed to eat your “regular meal,” try to make it representative of what you typically consume for breakfast or lunch, ensuring it contains at least 75 grams of carbohydrates as recommended by your lab or doctor in India. Avoid unusually large or high-sugar meals just for the test.
Accurate Timing:
This is perhaps the most critical aspect. Note the exact time you begin eating your meal, not when you finish. The second blood sample must be collected precisely two hours from that start time. Even a slight deviation can impact accuracy.
Avoiding Strenuous Activity:
During the 2-hour waiting period, avoid any vigorous exercise or physical exertion. Light activities like walking within your home or office are generally fine, but intense workouts can lower blood sugar, leading to a misleading result.
Medication Review:
Discuss all current medications, including over-the-counter drugs, supplements, and herbal remedies, with your doctor before the test. Some medications can influence blood sugar levels and may need to be adjusted or paused temporarily as advised by your physician.
Staying Hydrated:
Drink plenty of plain water throughout the day leading up to the test and during the waiting period. Dehydration can affect blood sugar readings.
Stress Management:
Try to minimize stress on the day of the test, as stress hormones can temporarily raise blood sugar.
By meticulously following these instructions, you empower your healthcare provider with the most accurate data to guide your diabetes management.
Strategies for Managing and Optimizing PPBS Levels
Taking control of your Post-Prandial Blood Sugar is a powerful step towards better diabetes management and a reduced risk of complications. It involves a holistic approach that integrates dietary changes, physical activity, medication adherence, and healthy lifestyle choices.
Dietary Interventions: The Cornerstone of PPBS Control
What you eat and how you eat it are the most significant factors influencing your PPBS.
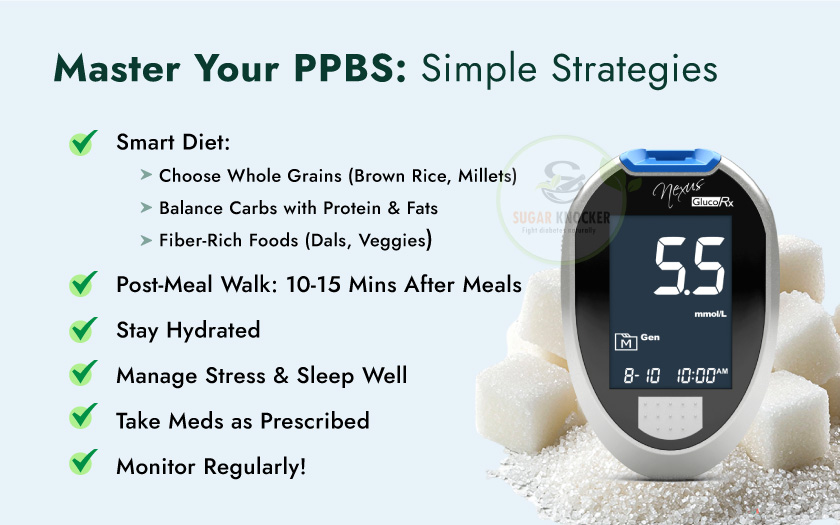
Carbohydrate Management:
- Understand Your Carbs: Focus on complex carbohydrates (found in whole grains, lentils, and many vegetables) which are digested slowly, leading to a gradual rise in blood sugar. Limit simple carbohydrates (like refined sugars, white bread, sugary drinks, and highly processed foods) that cause rapid and sharp spikes.
- Portion Control and Counting: Learn to estimate or count the carbohydrate content of your meals. Many individuals in India find success with systems like carbohydrate counting or portion exchange lists. A dietitian can provide personalized guidance on this.
- Embrace Fiber: Foods rich in dietary fiber (e.g., whole grains like oats, brown rice, jowar, bajra; pulses like dal and rajma; fruits with skin; and non-starchy vegetables) slow down the digestion and absorption of glucose, preventing rapid PPBS surges.
- Limit Refined Sugars and Processed Foods: These are notorious for causing dramatic blood sugar spikes. Read food labels carefully and minimize intake of sweets, pastries, sugary drinks, and packaged snacks.
Balanced Meals:
- Protein (e.g., paneer, lean meats, fish, eggs, pulses, tofu) and healthy fats (e.g., nuts, seeds, avocado, olive oil, mustard oil) help slow down gastric emptying, reducing the speed at which glucose enters the bloodstream and thereby mitigating sharp PPBS peaks.
- An ideal plate method, often recommended in India, involves filling half your plate with non-starchy vegetables, a quarter with protein, and a quarter with complex carbohydrates.
Meal Timing and Frequency:
- Regular Meals: Eating meals at consistent times helps regulate your body’s glucose response. Avoid skipping meals, as this can lead to overeating later and subsequent larger blood sugar spikes.
- Avoid Late-Night Heavy Meals: Eating heavy, carbohydrate-rich meals close to bedtime can result in elevated blood sugar overnight and into the morning.
Glycemic Index (GI) and Glycemic Load (GL):
- Glycemic Index (GI): This ranks carbohydrate-containing foods based on how quickly they raise blood sugar. Low GI foods (e.g., most vegetables, whole fruits, lentils) cause a slower, more gradual rise.
- Glycemic Load (GL): This considers both the GI of a food and the amount of carbohydrates in a typical serving. It’s a more comprehensive measure. Incorporating low-GI and low-GL foods into your diet can significantly help manage PPBS.
Regular Physical Activity:
Exercise is a powerful tool for managing PPBS and improving overall diabetes health.
- Improved Insulin Sensitivity: Physical activity helps your cells become more sensitive to insulin, meaning they can take up glucose more efficiently from the bloodstream.
- Glucose Uptake by Muscles: When you exercise, your muscles use glucose for energy, helping to lower blood sugar levels, even without the immediate presence of insulin.
- Recommendations: Aim for at least 150 minutes of moderate-intensity aerobic activity per week (e.g., brisk walking, cycling, swimming), spread over at least 3 days. Additionally, include 2-3 sessions per week of strength training (e.g., weightlifting, bodyweight exercises).
- Timing of Exercise: A short walk (10-15 minutes) after a meal can be particularly effective in blunting post-meal blood sugar spikes. This is a simple yet impactful habit.
Medication Adherence (if applicable):
If your doctor has prescribed diabetes medication (oral hypoglycemic agents or insulin), taking them exactly as directed is crucial for PPBS control.
- Different medications work in different ways to lower blood sugar, some specifically targeting post-meal spikes.
- Never adjust your medication dosage or schedule without consulting your doctor.
Weight Management:
Achieving and maintaining a healthy weight is fundamentally important for improving insulin sensitivity and, consequently, PPBS control. Even modest weight loss can make a significant difference.
Stress Management Techniques:
Chronic stress triggers the release of hormones like cortisol, which can elevate blood sugar levels. Incorporate stress-reducing activities into your daily routine:
- Meditation or mindfulness.
- Yoga or deep breathing exercises.
- Spending time in nature.
- Engaging in hobbies you enjoy.
Adequate Sleep:
Poor sleep quality and insufficient sleep can contribute to insulin resistance and higher blood sugar levels. Aim for 7-9 hours of quality sleep each night. Establish a consistent sleep schedule and create a relaxing bedtime routine.
Regular Monitoring:
Consistent at-home blood glucose monitoring, including PPBS checks, is your best guide. It helps you:
- Understand how different foods, activities, and stress levels affect your individual PPBS.
- Identify patterns and triggers for high or low blood sugar.
- Empower you to make immediate adjustments (e.g., a short walk after a heavy meal).
Professional Guidance:
Never underestimate the value of your healthcare team. Work closely with:
- Your Doctor/Endocrinologist: For medication adjustments, overall treatment plans, and addressing complications.
- Registered Dietitian or Nutritionist: For personalized meal planning, carbohydrate counting, and dietary strategies tailored to your needs and cultural preferences.
- Certified Diabetes Educator: For comprehensive guidance on all aspects of diabetes self-management.
By integrating these strategies, you can proactively manage your PPBS levels, leading to more stable blood sugar, reduced risk of complications, and an improved quality of life.
When PPBS Levels Are High or Low: What to Do?
Understanding what to do when your PPBS levels are outside your target range is crucial for immediate safety and long-term management.
Understanding High PPBS (Hyperglycemia):
High blood sugar after meals, or post-prandial hyperglycemia, means your body isn’t effectively clearing glucose from your bloodstream.
Causes:
- Too many carbohydrates: Consuming more carbohydrates than your body or medication can handle.
- Insufficient medication/insulin: Your current dose might not be adequate for the meal consumed.
- Stress or illness: Both can temporarily elevate blood sugar.
- Lack of physical activity: Especially after a meal.
- Insulin resistance: Your cells aren’t responding well to insulin.
- Incorrect medication timing: Taking medication too late relative to the start of the meal.
Symptoms:
- Increased thirst (polydipsia)
- Frequent urination (polyuria)
- Fatigue or lethargy
- Blurred vision
- Headache
- Feeling sluggish or unwell
Immediate Actions (The “Rule of 15” for conscious individuals):
- Consume 15 grams of fast-acting carbohydrates: This can be 3-4 glucose tablets, half a cup (120 ml) of fruit juice or regular soda (not diet), 1 tablespoon of sugar or honey, or 5-6 hard candies.
- Wait 15 minutes: Allow the carbohydrates to be absorbed.
- Re-check blood sugar: If it’s still below 70 mg/dL, repeat the 15 grams of fast-acting carbohydrates and wait another 15 minutes.
- Eat a small meal/snack: Once blood sugar is above 70 mg/dL, eat a small meal or snack containing both carbohydrates and protein (e.g., a small sandwich, a glass of milk and a biscuit) to prevent another drop.
Preventive Measures:
- Consistent Meal Times: Don’t skip meals, especially if you’re on medication.
- Carry Fast-Acting Carbs: Always have glucose tablets or a small juice box with you.
- Adjust Medication/Insulin: Discuss any recurring low blood sugar episodes with your doctor. They may need to adjust your medication.
- Monitor Blood Sugar Before Exercise: If you’re exercising intensely, you might need a small snack beforehand or a medication adjustment.
The Importance of Logging Readings:
Maintaining a detailed log of your PPBS readings, along with notes on what you ate, your activity levels, and any symptoms, is incredibly helpful. This data helps you and your healthcare team identify patterns, understand your body’s unique responses, and make more precise adjustments to your diabetes management plan.
Living with PPBS Awareness: Empowering Your Diabetes Journey
Understanding and actively managing your Post-Prandial Blood Sugar is not just about numbers on a meter; it’s about empowerment. It transforms diabetes management from a reactive process into a proactive journey.
Self-Monitoring as a Tool for Empowerment:
When you consistently check your PPBS, you gain invaluable insights into how your body responds to different foods, stress, and physical activity. This knowledge empowers you to:
- Make informed choices about your diet. You learn which foods cause significant spikes and which don’t, allowing you to tailor your meal plans effectively.
- Understand the immediate impact of exercise. A short walk after a meal, for example, can become a conscious strategy to manage your numbers.
- Recognize early warning signs of high or low blood sugar, enabling quicker and more effective intervention.
This self-awareness cultivates a sense of control over your condition, reducing feelings of helplessness and anxiety often associated with diabetes.
Working Collaboratively with Your Healthcare Team:
Your PPBS readings are a goldmine of information for your healthcare providers. Share your logs and observations regularly. This open communication allows your doctor, dietitian, and diabetes educator to:
- Fine-tune your medication, insulin dosages, and treatment plan with greater precision.
- Provide personalized dietary advice, helping you navigate Indian cuisine and meal patterns for optimal blood sugar control.
- Offer strategies for incorporating physical activity into your daily life that align with your PPBS goals.
- Address any challenges or concerns you face, ensuring you have the support you need.
Remember, you are an active partner in your diabetes care, and your insights are crucial for effective management.
Setting Realistic Goals:
While striving for optimal PPBS numbers is important, it’s equally important to set realistic goals. Diabetes management is an ongoing process, and occasional fluctuations are normal. Focus on consistent effort and continuous learning rather than striving for “perfect” numbers every single time. Discuss achievable targets with your doctor that align with your lifestyle and overall health.
Staying Informed and Adaptable:
The field of diabetes management is constantly evolving. Staying informed about new research, technologies (like continuous glucose monitors), and treatment approaches can further empower your journey. Be open to adapting your strategies as your body changes, or as new tools become available.
Celebrating Small Victories:
Managing diabetes is a marathon, not a sprint. Acknowledge and celebrate your progress, no matter how small. Did you successfully keep your PPBS within range after a challenging meal? Did you make a conscious choice to walk after dinner? These small victories build confidence and reinforce positive habits, fueling your motivation for continued self-care.
By embracing PPBS awareness, you transform from a passive recipient of medical advice into an empowered individual actively steering your diabetes journey towards better health and well-being.
What does PPBS stand for and why is it important in diabetes management?
PPBS stands for Post-Prandial Blood Sugar. It refers to your blood sugar level measured typically 2 hours after you start eating a meal. It’s crucial because it reveals how effectively your body processes carbohydrates from food. High PPBS, even with normal fasting sugar, significantly increases your risk of long-term diabetes complications like heart disease, kidney damage, and nerve damage. It also serves as an early indicator for prediabetes.
What are the normal PPBS levels, and what are the target levels for people with diabetes in India?
For individuals without diabetes, a normal PPBS level (2 hours after a meal) is generally below 140 mg/dL. For those with diagnosed diabetes, the target PPBS level is usually below 180 mg/dL 2 hours after a meal. However, your doctor will set a personalized target based on your health condition, age, and other factors.
How is the PPBS test performed, and what preparation is required?
The PPBS test usually involves taking a blood sample exactly 2 hours after you begin eating a specific meal (either a standardized glucose solution or a regular meal as instructed by your doctor). If a fasting sample is also required, you’ll need to fast for 8-12 hours beforehand. It’s crucial to note the exact start time of your meal and avoid any strenuous physical activity or consuming anything other than water during the 2-hour waiting period. Discuss all your medications with your doctor before the test.
Can my PPBS be high even if my fasting blood sugar is normal?
Yes, absolutely! This is a common scenario, especially in the early stages of prediabetes or Type 2 Diabetes. Your body might manage fasting glucose well, but struggle to process the sudden influx of sugar after a meal, leading to significant spikes in PPBS. This is why monitoring PPBS provides a more complete picture of your blood sugar control.
What Indian foods commonly cause high PPBS spikes, and what are better alternatives?
Foods high in refined carbohydrates and simple sugars are major culprits. This includes white rice, white bread, pastries, sugary drinks, potato, and many traditional sweets like Jalebi, Gulab Jamun, etc. Better alternatives include:
Whole grains: Brown rice, millets (bajra, ragi, jowar), whole wheat roti/chapati instead of white rice or refined flour bread.
High-fiber options: Plenty of dals, legumes, vegetables, and whole fruits.
Balanced meals: Combining carbohydrates with protein (paneer, dal, lean meats, eggs) and healthy fats to slow down glucose absorption.Does exercise help in controlling PPBS? What kind and when?
Yes, regular physical activity is highly effective! Exercise increases insulin sensitivity and helps your muscles use glucose for energy, thereby lowering blood sugar. Even a short, gentle walk (10-15 minutes) immediately after your main meals can significantly help blunt post-meal blood sugar spikes. Aim for at least 150 minutes of moderate-intensity exercise per week, combined with strength training.
How does stress affect my PPBS levels?
Chronic stress can significantly impact your blood sugar. When you’re stressed, your body releases hormones like cortisol, which can increase insulin resistance and raise blood glucose levels, including PPBS. Incorporating stress-management techniques like yoga, meditation, or deep breathing can be beneficial for overall blood sugar control.
My PPBS is consistently high; what should I do?
If your PPBS readings are consistently high, the first step is to consult your doctor or endocrinologist. They may recommend:
Reviewing and adjusting your current medication or insulin dosage.
Referring you to a registered dietitian for a personalized meal plan and carbohydrate counting guidance.
Discussing lifestyle changes, including diet, exercise, and stress management.
More frequent blood sugar monitoring to identify patterns.Can lifestyle changes alone help manage high PPBS, or do I always need medication?
For individuals with prediabetes or early-stage Type 2 Diabetes, significant lifestyle changes – including a balanced diet rich in fiber, regular physical activity (especially post-meal walks), weight management, and stress reduction – can often normalize PPBS levels and even prevent or delay the need for medication. However, for many with established diabetes, medication is a necessary component alongside lifestyle changes. Always discuss the best approach with your doctor.
How often should I check my PPBS, and should I log the readings?
The frequency of PPBS monitoring depends on your individual condition and your doctor’s recommendation. If you have diabetes, your doctor might ask you to check it regularly (e.g., a few times a week, or more frequently if starting new medication). Yes, logging your readings (along with notes on what you ate, activity, and medication) is extremely helpful. This data helps you and your healthcare team identify patterns, understand your body’s unique responses, and make more precise adjustments to your diabetes management.
Conclusion: Taking Control of Your Post-Meal Health
The surge in interest around Post-Prandial Blood Sugar (PPBS) in diabetes is a testament to its critical role in effective management. We’ve journeyed through its definition, highlighted its profound importance in detecting and preventing complications, understood what the numbers mean, and outlined the steps for accurate testing. Most importantly, we’ve explored a comprehensive array of strategies – from mindful eating and regular physical activity to medication adherence and stress management – all designed to help you optimize your post-meal glucose levels.
PPBS is no longer just a secondary metric; it’s a vital indicator that offers invaluable, real-time insights into how your body handles food. It completes the picture that fasting glucose and HbA1c provide, enabling a more precise and personalized approach to diabetes care. Ignoring those post-meal spikes can have silent, long-term consequences, but by actively monitoring and managing them, you significantly reduce your risk of serious complications like heart disease, nerve damage, and kidney issues.
Empower yourself by understanding your PPBS. Discuss this critical test with your doctor, work with a dietitian to tailor your meals, and embrace the power of a healthy, active lifestyle. Remember, every conscious choice you make regarding your diet and daily habits has a direct impact on your post-meal blood sugar.
Taking control of your PPBS is a powerful, proactive step towards a healthier, more fulfilling future. It’s about more than just managing a condition; it’s about unlocking better health, one meal at a time.